pCR rates were similar for patients treated with [Ogivri] compared with [Herceptin] in our real-world study of HER2+ neoadjuvant [early breast cancer] and comparable to pivotal phase 3 trials.
- Bone Health
- Immunology
- Hematology
- Respiratory
- Dermatology
- Diabetes
- Gastroenterology
- Neurology
- Oncology
- Ophthalmology
- Rare Disease
- Rheumatology
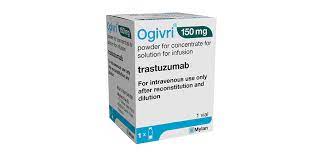
Ogivri Equivalence Demonstrated in Neoadjuvant HER2+ Comparative Trial
Investigators further elucidate the equivalence of a trastuzumab biosimilar vs Herceptin in human epidermal growth factor receptor 2–positive (HER2+) breast cancer.
Investigators in Alberta, Canada, said no significant differences in pathologic complete response rates (pCRs) were observed in a study of patients with human epidermal growth factor receptor 2–positive (HER2+) treated with the biosimilar trastuzumab Ogivri vs the originator product, Herceptin.
The study authors postulated that although biosimilars are certified as having no clinically meaningful differences from originator products, there is potential for clinically meaningful differences in outcomes because biosimilar manufacturers must produce new cell lines to replicate originator biologics and are not given access to the originator cell lines.
Concerns about “this inherent alteration in production” are settled through phase 1 pharmacokinetic and pharmacodynamic comparative studies and phase 3 studies to demonstrate biosimilar equivalency in patients for at least 1 indication of the originator product, investigators said.
Prior confirmatory studies have evaluated the biosimilarity of Ogivri and Herceptin in the metastatic HER2+ setting. In this study, investigators sought to elucidate biosimilar equivalence in the neoadjuvant, or early breast cancer (EBC), setting.
The study enrolled patients (N = 136; 56% originator, 43% biosimilar) treated with trastuzumab originator from November 2018 to October 2019 and the biosimilar from December 2019 to September 2020. There was no crossover between products. Investigators used logistic regression to control for factors that might affect pCR in either cohort, such as biosimilar or originator agent, age, tumor type, node positivity, tumor grade, hormone receptor status, treatment with chemotherapy, and whether chemotherapy treatment was completed.
Based on the logistic regression model, investigators saw no significant difference in pCR odds for patients treated with biosimilar vs originator (odds ratio [OR], 1.1; 95% CI, 0.5-2.4; P = .85). However, there was a statistically insignificant lower likelihood of pCR in patients with anthracycline use (OR, 0.72; 95% CI, 0.3-1.6; P = .417).
Investigators observed no significant differences in baseline characteristics among patients except the proportion of those with node negative results: 39%, biosimilar; 14.3%, originator (P = .001). For patients treated with biosimilar vs originator, pCR was a nonstatistically significant 35.6% vs 40.3%, respectively (P = .598).
“pCR rates were similar for patients treated with [Ogivri] compared with [Herceptin] in our real-world study of HER2+ neoadjuvant EBC and comparable to pivotal phase 3 trials,” the authors concluded.
Reference
Yang C, Khwaja R, King K, et al. Trastuzumab-dkst versus trastuzumab: real-world pCR rates in patients with HER2+ breast cancer treated with neoadjuvant chemotherapy plus trastuzumab from Alberta, Canada. Presented at: ASCO 2021; June 3-7, 2021. Abstract e12569.
Newsletter
Where clinical, regulatory, and economic perspectives converge—sign up for Center for Biosimilars® emails to get expert insights on emerging treatment paradigms, biosimilar policy, and real-world outcomes that shape patient care.