- Bone Health
- Immunology
- Hematology
- Respiratory
- Dermatology
- Diabetes
- Gastroenterology
- Neurology
- Oncology
- Ophthalmology
- Rare Disease
- Rheumatology
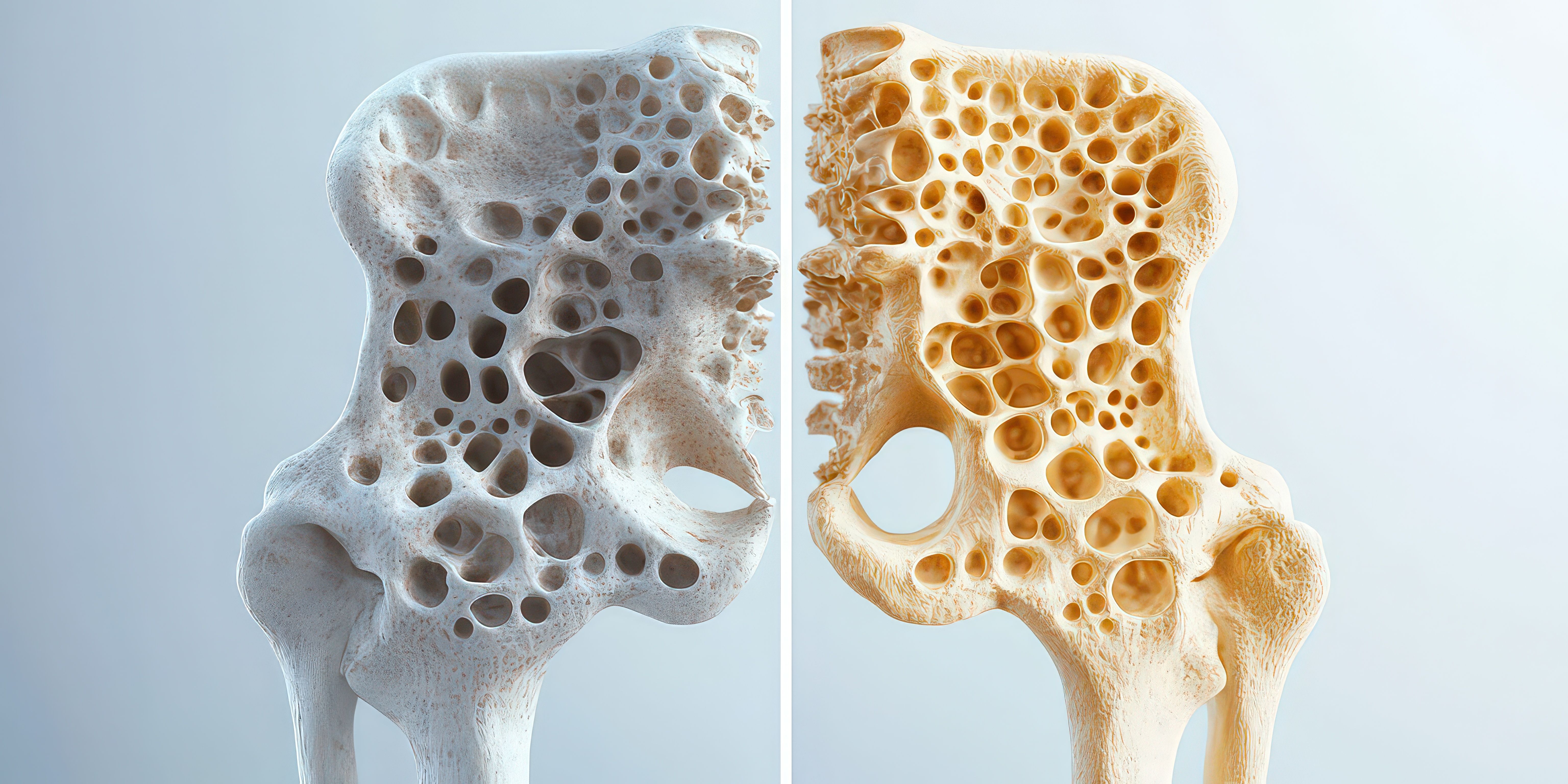
Trial Data Support Equivalence of Denosumab Biosimilar in Postmenopausal Osteoporosis
Denosumab biosimilars enhance treatment access for postmenopausal osteoporosis, demonstrating equivalent efficacy and safety to reference products in recent trials.
As biosimilars move into broader therapeutic areas, osteoporosis has emerged as a key test case for demonstrating equivalence in both bone density outcomes and safety.
Denosumab biosimilars enhance treatment access for postmenopausal osteoporosis, demonstrating equivalent efficacy and safety to reference products in recent trials. | Image credit: Lamina - stock.adobe.com
With 9 and 10 pairs of denosumab biosimilars approved in the US and European Union, respectively, lower-cost biologic alternatives to Prolia and Xgeva (reference denosumab) are increasingly shaping treatment access in osteoporosis, where long-term adherence is essential to prevent fractures and downstream costs.1
In a recent randomized phase 3 trial, investigators addressed persistent cost and access barriers associated with denosumab, a monoclonal antibody that inhibits receptor activator of nuclear factor-κB ligand (RANKL) and is widely used for fracture risk reduction.2 Although denosumab has demonstrated durable efficacy and an acceptable long-term benefit–risk profile, its biologic pricing has limited uptake in some settings. Biosimilars are intended to expand access while maintaining equivalent clinical performance, a requirement emphasized by both the FDA and the European Medicines Agency.
The multicenter, double-blind study enrolled women aged 60 to 90 years with postmenopausal osteoporosis across 76 sites in Europe and the US between 2021 and 2023. Participants were randomized 1:1 to receive either the proposed biosimilar RGB-14-P or reference denosumab at a dose of 60 mg administered subcutaneously every 6 months, with follow-up through 52 weeks. All participants also received daily calcium and vitamin D supplementation.
A total of 473 participants were randomized and treated (n = 242 assigned to RGB-14-P and 231 to reference denosumab), and more than 92% completed the 52-week main study period. At baseline, the mean age was 66.7 years, and nearly all participants were White. Mean lumbar spine bone mineral density (BMD) T-scores were approximately −3.0 in both groups, consistent with established osteoporosis. Around 10% of participants in each arm had experienced a fracture within the year prior to enrollment.
The trial included 2 co-primary end points designed to satisfy regulatory expectations for biosimilar equivalence: percentage change from baseline in lumbar spine BMD at week 52 and area under the effect curve for percentage change in serum C-terminal telopeptide of type 1 collagen (CTX) through week 26. Both end points met prespecified equivalence margins.
At week 52, the adjusted mean increase in lumbar spine BMD was 4.89% in the biosimilar group and 4.55% in the reference denosumab group, yielding an estimated between-group difference of 0.34 percentage points (95% CI, −0.40 to 1.09), well within the equivalence margin of ±1.45%. Analyses required by US regulators also demonstrated noninferiority and nonsuperiority of the biosimilar relative to the reference product.
Pharmacodynamic outcomes mirrored these findings. The geometric mean ratio for the CTX area-under-the-curve end point was 1.01 (95% CI, 0.98-1.05; P = .49), confirming equivalent suppression of bone resorption. Secondary efficacy end points, including changes in total hip and femoral neck BMD at weeks 26 and 52, did not differ significantly between treatment arms.
Fracture outcomes, although not powered as primary end points, were similar across groups. By week 52, vertebral fragility fractures occurred in 1.7% of participants receiving RGB-14-P and 3.5% of those receiving reference denosumab, while nonvertebral fragility fractures occurred in 1.7% and 4.3%, respectively. Investigators noted that the overall fracture incidence was low, a common limitation in osteoporosis trials of relatively short duration.
Immunogenicity rates were low and comparable. Binding antidrug antibodies were detected in fewer than 1% of participants in either group, and neutralizing antibodies were identified in 0.4% of participants in each arm. Safety profiles were also similar, with approximately two-thirds of participants in each group experiencing at least 1 treatment-emergent adverse event. The most commonly reported events included infections such as COVID-19 and nasopharyngitis, hypocalcemia, headache, and arthralgia. Serious adverse events were uncommon and balanced between groups.
Investigators emphasized that the findings align with regulatory standards for biosimilar development. They wrote that the biosimilar “demonstrated equivalent efficacy and pharmacodynamics and similar immunogenicity and safety” compared with reference denosumab, adding that the results support its ability to “replicate the therapeutic benefit” of the originator in clinical practice.
Several limitations were acknowledged. The study population lacked racial diversity, which may affect generalizability, and follow-up was limited to 1 year, precluding assessment of longer-term fracture outcomes. Additionally, low fracture event rates constrained conclusions regarding comparative fracture prevention, although BMD changes are an accepted surrogate end point for regulatory decision-making.
From a managed care perspective, the results add to a growing body of evidence supporting denosumab biosimilars as clinically comparable options that may reduce drug spending while preserving outcomes. If approved and priced competitively, RGB-14-P could provide payers and health systems with additional leverage to improve access and support sustained osteoporosis treatment adherence.
References
- Biosimilars approvals. The Center for Biosimilars®. Updated December 22, 2025. Accessed January 15, 2026. https://www.centerforbiosimilars.com/biosimilar-approvals
- Seefried L, Ferrari S, Páll D, et al. A randomised phase 3 study comparing the efficacy and safety of proposed denosumab biosimilar RGB-14-P and reference denosumab in women with postmenopausal osteoporosis. Osteoporos Int. 2025;36(12):2497-2507. doi:10.1007/s00198-025-07711-x
Newsletter
Where clinical, regulatory, and economic perspectives converge—sign up for Center for Biosimilars® emails to get expert insights on emerging treatment paradigms, biosimilar policy, and real-world outcomes that shape patient care.
