- Bone Health
- Immunology
- Hematology
- Respiratory
- Dermatology
- Diabetes
- Gastroenterology
- Neurology
- Oncology
- Ophthalmology
- Rare Disease
- Rheumatology
Part 2: French Study Finds Trastuzumab Biosimilar Program Could Generate Meaningful Savings
In part 2 of a 3-part series for Global Biosimilars Week, The Center for Biosimilars® explores a cost-effectiveness analysis evaluating the use of subcutaneous trastuzumab biosimilars to treat breast cancer in a French hospital setting.
Click to enlarge.
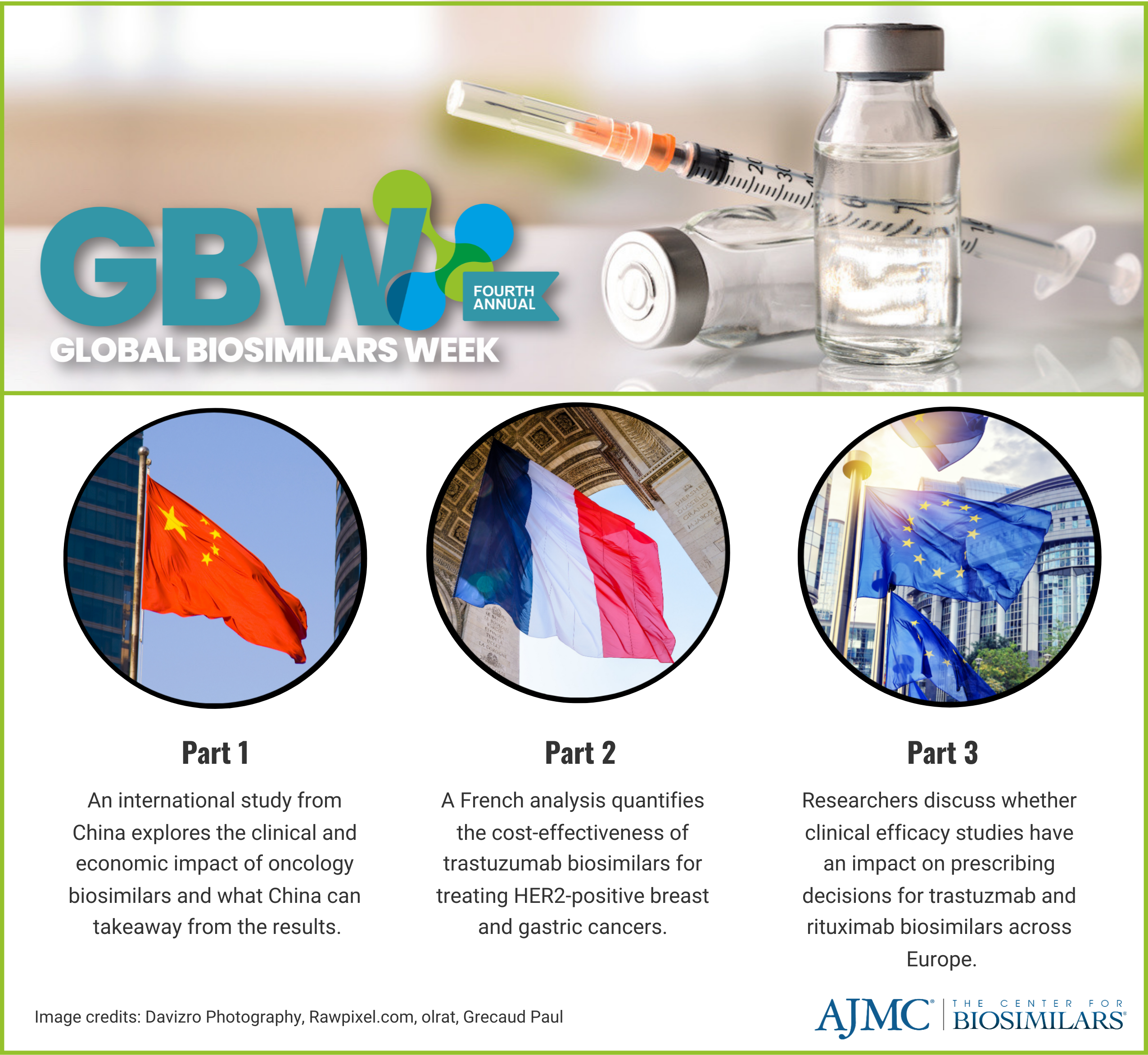
In part 2 of a 3-part series for Global Biosimilars Week, The Center for Biosimilars® explores a cost-effectiveness analysis evaluating the use of subcutaneous (SC) and intravenous (IV) trastuzumab products to treat breast cancer in a French hospital setting.
Global Biosimilars Week is an annual awareness campaign created by the International Generic and Biosimilar Medicines Association. The event runs from November 13-17, 2023 and serves as a way to expand awareness of biosimilars, their clinical effects compared to originators, the economic impacts of using them, and the growing industry worldwide. To read part 1, click here. To read part 3, click here.
In the present analysis, published in The Breast, researchers found that the implementation of a trastuzumab programs that prioritizes the use of the SC version of reference trastuzumab (Herceptin) and EMA-approved IV trastuzumab biosimilars (Kanjinti, Ogivri, Ontruzant, Herzuma, Trazimera) is cost-effective for French hospital systems.
Researchers collected data from a French Diagnostic Related Groups (French DRG) database. The study period was set at 1 year (2019), encompassing 18 cycles of trastuzumab administration at 3-week intervals. The study population included 544 patients with HER2-positive breast cancer from Normandy France.
Two simulations were evaluated:
- Simulation 1: use of IV trastuzumab biosimilar to replace IV and SC reference trastuzumab
- Simulation 2: use of SC reference trastuzumab to replace IV reference trastuzumab
The cost of stay was based on the cost of consumables related to the route of trastuzumab administration (SC vs IV), the time patients spent with health care professionals, and the type of chemotherapy that was administered to patients receiving trastuzumab.
Simulation 1 revealed that the use of an IV trastuzumab biosimilar in combination with IV chemotherapy led to a cost saving of €11,889, amounting to €12 per patient per year and a 14% a 60% cost reduction compared to the current situation. However, this simulation also showed an increase in the length of chemotherapy sessions compared with the current time (10 minutes per patient per year).
Simulation 2 demonstrated that the use of SC reference trastuzumab (in monotherapy) generated €15,376 in cost savings (€51 per patient per year), a 60% cost reduction compared with the current situation. This simulation also resulted in a time saving of 68 and 78 minutes per patient per year compared to the current situation and simulation 1, respectively.
The simulations had different impacts on productivity. In Simulation 1, the impact was mainly due to the time of administration of SC reference trastuzumab in combination IV chemotherapy. The study estimated that the maximum difference between the groups (IV biosimilar/IV chemotherapy and SC reference product/IV chemotherapy) could be 21 min.
In Simulation 2, the impact on productivity earning potential was mainly due to the time saving relative to the SC administration of trastuzumab in monotherapy, which is unlikely to vary over time. The study found that the productivity earning potential was the factor that caused the most variation in Simulation 2, with a variation in results (±27%) greater than the variation in the productivity parameter (±20%).
The study has limitations: it didn't evaluate the direct impact or costs of a biosimilar incentive program, lacked specific day hospital cost data, and relied on accurate coding for French DRG information. Moreover, it focused solely on a hospital perspective, neglecting a broader societal viewpoint for a comprehensive cost-effectiveness analysis of trastuzumab biosimilars versus original drugs.
Reference
Barat EC, Arrii MLE, Soubieux-Bourbon A, Daouphars M, Varin R, Tilleul PR. Cost effectiveness of using trastuzumab biosimilars compared to trastuzumab original drugs to treat breast cancer in a hospital setting. Breast. Published online October 11, 2023. doi:10.1016/j.breast.2023.103588
Newsletter
Where clinical, regulatory, and economic perspectives converge—sign up for Center for Biosimilars® emails to get expert insights on emerging treatment paradigms, biosimilar policy, and real-world outcomes that shape patient care.
