- Bone Health
- Immunology
- Hematology
- Respiratory
- Dermatology
- Diabetes
- Gastroenterology
- Neurology
- Oncology
- Ophthalmology
- Rare Disease
- Rheumatology
Proposed Bevacizumab Biosimilar Demonstrates Clinical Equivalence to Avastin in NSCLC
The proposed bevacizumab biosimilar BAT1706 (Bio-Thera Solutions) demonstrated equivalence to the reference product (Avastin) in a phase 3 comparative efficacy trial in patients with advanced nonsquamous non–small cell lung cancer (NSCLC).
Image credit: Dr_Microbe - stock.adobe.com
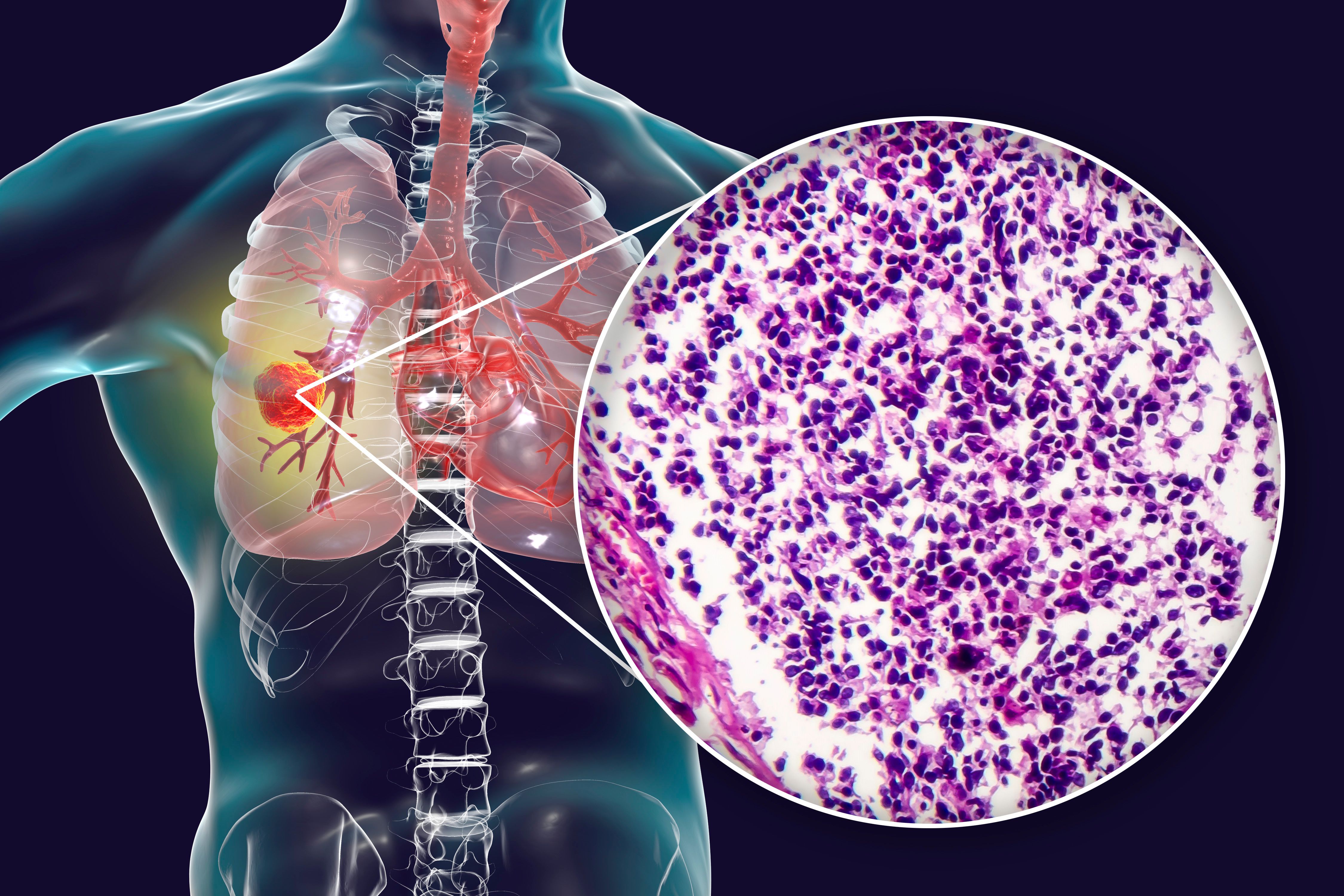
The proposed bevacizumab biosimilar BAT1706 (Bio-Thera Solutions) demonstrated equivalence to the reference product (Avastin) in a phase 3 comparative efficacy trial in patients with advanced nonsquamous non–small cell lung cancer (NSCLC).
Lung cancer is the most common cause of death from cancer worldwide and is responsible for more than 20% of cancer deaths in China, according to the authors of the study. The majority of lung cancers are NSCLC.
Inhibition of angiogenesis via biologics targeting vascular endothelial growth factor (VEGF) aims to prevent the formation of new blood vessels in a variety of solid tumor types, including NSCLC. Bevacizumab, a monoclonal antibody targeting VEGF, combined with paclitaxel and carboplatin chemotherapy has been approved as a first‐line treatment for late‐stage NSCLC since 2006 in the US, 2007 in the EU, and 2015 in China.
The candidate bevacizumab biosimilar BAT1706 has demonstrated analytical similarity to the reference product and pharmacokinetic similarity in healthy participants. The current study compared the efficacy and safety of BAT1706 to the EU-sourced reference bevacizumab in combination with chemotherapy in patients with advanced nonsquamous NSCLC.
The multicenter trial in China included 651 patients, 325 in the biosimilar group and 326 in the reference product group. The patients received 6 cycles of paclitaxel and carboplatin chemotherapy along with either biosimilar or reference bevacizumab every 3 weeks, followed by maintenance therapy with either biosimilar or reference bevacizumab. The authors noted that demographic and baseline characteristics were similar between the treatment arms, and at the data cutoff date, exposure to BAT1706 and the EU-source reference bevacizumab were similar, as were the median number of carboplatin infusions.
The primary endpoint of the trial was overall response rate at week 18 (ORR18). Clinical equivalence was evaluated based on the equivalence margins defined by China’s National Medical Products Administration, FDA, and the European Medicines Agency (EMA). In the US and China (NMPA), the 90% CI of the ratio of ORR18 between groups must be within 0.75-1.33 and 0.73-1.36, respectively. For the EMA, clinical equivalence is defined by the 95% CI of the difference in ORR18 between groups within the margin of –0.12 to 0.15. The ORR18 was 48% in the biosimilar group and 44.5% in the reference product group. The ratio (1.08; 90% CI, 0.94-1.24) and difference (0.03; 95% CI, –0.04 to 0.11) in ORR18 between groups met the equivalence criteria defined by the NMPA, FDA, and EMA.
According to the authors, secondary endpoints including progression-free survival (PFS), overall survival (OS), duration of response (DoR), and ORR at 6 months (ORR6) were comparable between groups. Median PFS was 8.1 months in the biosimilar group and 7.7 months in the reference product group, median OS was 16.4 months and 18.5 months, median DoR was 6.9 months and 7.1 months, and ORR after 6 weeks was 27% and 23%. They noted that their efficacy results were consistent with previously published phase 2 and 3 data on bevacizumab used in combination with carboplatin and paclitaxel for advanced NSCLC.
At the time of data cutoff, 66% of patients had stopped treatment. The most common reasons were disease progression, treatment-emergent adverse events (TEAEs), death, and withdrawal of consent. According to the authors, “the safety profile of BAT1706 was consistent with that of EU‐bevacizumab and no new safety signals were observed.”
The incidence of TEAEs was similar between groups, with 97% and 98% of patients in the biosimilar and reference product groups experiencing at least 1 TEAE. Of those, over half (60% and 58%) of patients had TEAEs related to bevacizumab. About one-third of patients (31%) reported at least 1 serious TEAE, and 10% and 9% of serious TEAEs in the biosimilar and reference product groups were related to bevacizumab. Carboplatin- and paclitaxel-related TEAEs also occurred at similar rates between groups. TEAEs leading to death that were considered related to bevacizumab occurred in 8 patients in the biosimilar group and 3 in the reference product group (5% of patients overall). TEAEs leading to discontinuation of treatment occurred in 28 patients in the biosimilar group and 25 in the reference product group (8% overall).
Regarding pharmacokinetics, the authors reported that mean serum concentrations of bevacizumab were comparable between groups throughout the study. Immunogenicity was also reported to be comparable between groups. Positive anti-drug antibody results following a negative result at baseline were detected in 12 patients in the biosimilar group and 10 in the reference product group.
Overall, the authors concluded that BAT1706 demonstrated clinical equivalence to the EU-sourced reference bevacizumab in efficacy, safety, pharmacokinetics, and immunogenicity when administered in combination with paclitaxel and carboplatin in patients with advanced nonsquamous NSCLC. They added, “these data add to the totality of evidence that BAT1706 is similar to reference bevacizumab.”
Reference
Chen L, Rangel JDG, Cil T, et al. Efficacy and safety of the proposed bevacizumab biosimilar BAT1706 compared with reference bevacizumab in patients with advanced nonsquamous non-small cell lung cancer: A randomized, double-blind, phase III study. Cancer Med. 2023;12(22):20847-20863. doi:10.1002/cam4.6664
Newsletter
Where clinical, regulatory, and economic perspectives converge—sign up for Center for Biosimilars® emails to get expert insights on emerging treatment paradigms, biosimilar policy, and real-world outcomes that shape patient care.
